When Dr. Stephanie Martin heard the urgent “Code Blue” message over the hospital intercom, she rushed to the aid of 34-year-old Tracy Hermanstorfer, who was in labor, but not in a good way. Martin knew that a Code Blue message meant it was something serious, and it just happened to be Christmas Eve.
It was lunchtime when the Code Blue came through. Dr. Martin rushed to the room of Hermanstorfer at the Memorial Hospital Central in Colorado Springs where she was on shift. She was lucky to have arrived just in the nick of time, but quickly realized it may have been too late…
Lunchtime
Most of the hospital staff were winding down as it was Christmas time, with a skeleton crew of staff on hand for emergencies. It was lunchtime on Christmas Eve when Martin was conferring with a patient in her office when suddenly the Code Blue came through on the intercom.
Ballroom Dancer
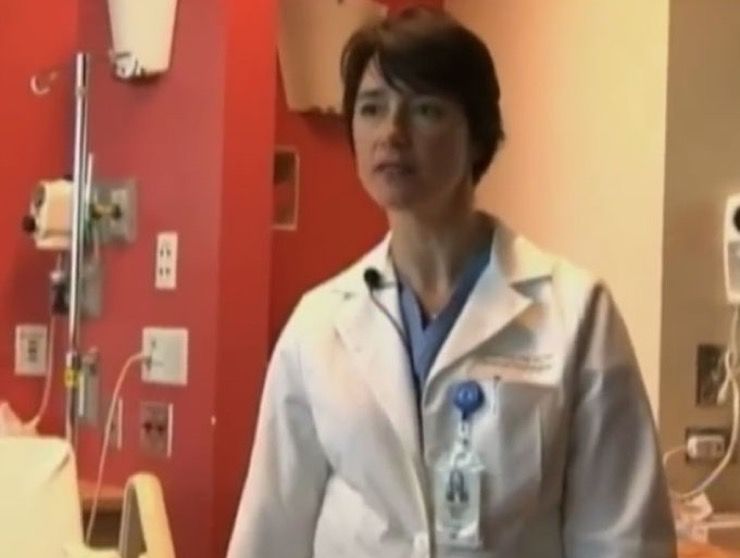
At the age of 42, Martin looks more like a ballerina in scrubs than the head of high-risk obstetrics at the hospital. In her spare time, Martin is a competitive ballroom dancer, and her physique and energy levels make her an ace doctor to boot. When the Code Blue came in, Martin arrived at the emergency within two minutes.
Code Blue
A Code Blue is an emergency announced in a hospital or medical facility whereby a patient in cardiopulmonary arrest requires the immediate assistance of a team of providers, often called a “Code Team,” who rush to the specific location of the patient to begin immediate resuscitative efforts. When Martin heard the person needing the help was in labor, she feared for the worst.
East Tower
The patient in danger, Hermanstorfer, was located in a room in the East Tower of the hospital. When the call over the intercom came: “Code blue, East Tower, labor and delivery rooms,” Martin ran down the hall to the room. “I can’t lose anyone on Christmas Eve,” she said to herself. But the situation was desperate, and both mother and baby were in dire straits.
Good Health
When Hermanstorfer arrived at her hospital with her husband Mike, a long-haul truck driver, earlier in the day she was in good health and expecting a normal delivery for her baby. She had given birth twice before and knew more or less what to expect once at the hospital. The mother-to-be and Mike were excited to be having a Christmas baby and knowing he was a boy they had already decided on a name.
Contractions Begin
When Hermanstorfer began to realize she was having contractions, she made her way to the hospital, arriving at around 12:30 in the afternoon. After a few hours of contractions, the pregnant woman was growing tired and decided to accept an epidural injection to ease the pain of labor and delivery. The baby’s heart rate was slow, but no major issues were noted at the time.
Long Day
Mike was playing the role of the perfect husband on that day as he attended to his wife’s every need and doted on her. Mike knew his wife was facing a long day ahead and wanted to offer her some words of comfort. “Rest, close your eyes,” Mike told her. “It looks like you’re going to have a long day.” But nobody could have predicted what happened next.
Previous Experience
As she raced to the Code Blue emergency, Martin recalled the Fourth of July 1997, which was the first time she worked as a physician on a maternity ward. On that day, Martin encountered a normal birth involving a 21-year-old woman, but things went wrong on that occasion. Amniotic fluid had escaped the placenta and entered the mother’s bloodstream, causing an allergic reaction. Both the mother and the baby died during that incident, and it left a deep and lasting impression on Martin.
Emotional Tailspin
Being that she was new at the job despite all her years of training, the incident sent Martin into an emotional tailspin. She found herself depressed and bedridden for days at a time, and no one could talk her out of her mood. It took Martin weeks to recover from that, and she said to herself, “I can’t give up. I have to find a solution,” according to a Gazette report.
Expert Skills
Having worked with maternal cardiac arrests for twelve years since the fateful July fourth incident, Martin became an expert in her field and just the person one would want around in such a situation. When Hermanstorfer closed her eyes and began to doze off, her husband felt that her hands were unusually cold and noticed her lips were turning blue. “What’s going on?” he asked a nurse in the room.
Saving Life
The nurse realized something was very wrong, and that’s when she pulled the Code Blue cord in the room. Mike was ushered into a corridor where two chaplains were waiting for him. He rushed back into the room where his wife was, noticing she wasn’t breathing and was in cardiac arrest. Mike prayed, hoping that his wife and son weren’t dead.
Many Causes
Hermanstorfer’s condition could have been caused by any number of factors. It could have been an amniotic embolism, an allergic reaction to the epidural. For that matter, it could have been down to a spontaneous irregular heartbeat, or the placenta separating from the uterus. In such situations protocol calls for the baby to be delivered before the mother is resuscitated.
Improving Chances
Through her years of experience, Martin knew that if there was any chance of saving the distressed mother, the fetus and placenta needed to be removed as soon as possible in order to take the strain off the mother’s heart. As two teams worked to save the patients – one team working on Hermanstorfer and the other standing ready to revive the baby – the atmosphere in the room was tangible.
Fading Heartbeat
When Martin noticed from the monitor that the baby’s heartbeat was fading fast, she instructed medical staff to intubate the mother, forcing air into her lungs with a manual pump so that the baby could get enough oxygen. Martin then planned to perform a C-section then and there and without hesitation.
C-Section Time
Martin had done them numerous times before, but when she poured a bottle of surgical soap over Tracy’s abdomen and made the first six-inch horizontal incision, she noted there was no blood as Tracy’s heart had stopped beating. The second cut was also horizontal and opened the uterus as intended. Martin pulled the baby from the amniotic fluid, lifted out the limp body and cut the umbilical cord.
Vital Functions
Martin immediately noticed that the baby’s vital functions were depressed. The boy was pale and not moving, so the doctor handed him to the neonatologist, who took the baby to the warming table. The baby’s nose and mouth were suctioned, and artificial respiration was applied. The baby had been delivered inside just five minutes, but things weren’t looking good.
Tiny Heartbeat
Martin was almost sure that the mother wouldn’t make it but was nicely surprised when she placed her finger on Hermanstorfer’s aorta and felt a tiny heartbeat. “Let’s get her to the operating room. Now!” she shouted. As Hermanstorfer was rushed on a gurney to the OR, she passed by her husband, Mike. Martin instructed him to “give her a kiss,” knowing it may be the last one he ever gave her.
Breathing Machine
Tracy Hermanstorfer was still very much alive, and her heartbeat was improving nicely. She was put on an automatic breathing machine to assist her as Martin removed the placenta and stitched the patient up. Hermanstorfer had survived and was taken to the ICU to recovery. Suddenly she awoke exclaiming, “My baby’s name is Coltyn.” Then Mike was summoned into a room by a nurse.
Feeling Proud
As soon as Mike had entered the room his baby son was thrust into his arms by the nurse. The baby seemed lifeless to Mike, but he was simply exhausted from the ordeal he had just been through. “He came alive in my arms,” Mike said. He was then taken to the ICU with the baby to be reunited with his wife.
Appreciating Life
Having made a full recovery, Tracy Hermanstorfer loves her son and is thrilled that he was saved. She told reporters that the near-death experience had taught her a lesson in appreciating life to the full and enjoying her three children. To Mike’s mind, the whole thing was a miracle, especially as doctors still have no idea what caused the emergency medical situation in the first place.