When 27-year-old Naomi Williams fell sick in the middle of the night, her partner Michael Lampe who was also the father of her unborn child, assumed she was just suffering from some pregnancy pangs as she was already six months down the line.
Lampe wasn’t overly worried about his partner’s well-being, as she drove herself alone to the emergency department of the local hospital in the Australian country town of Tumut. When she began to vomit and experienced head and back pains, Williams decided to go and get it checked out.
Nothing Serious
Having arrived at the emergency room, Williams was barely able to get out of her car and make it inside. She felt disoriented, sweaty and was suffering from flu-like symptoms. According to the hospital report, Williams was only there for 34 minutes before nurses gave her Panadol and told her to go home. But tragedy was just around the corner.
Later On
Williams listened to the medical advice and drove back home. Just fifteen hours later and Williams would find herself being rushed back to the hospital, but this time it was for a cardiac arrest she was going through. She suffered the heart attack while in the back of the ambulance which had been caused by sepsis from a nasty bacterial infection. The EMT staff knew that Williams wasn’t looking good, but they never expected what happened next.
Total Shock
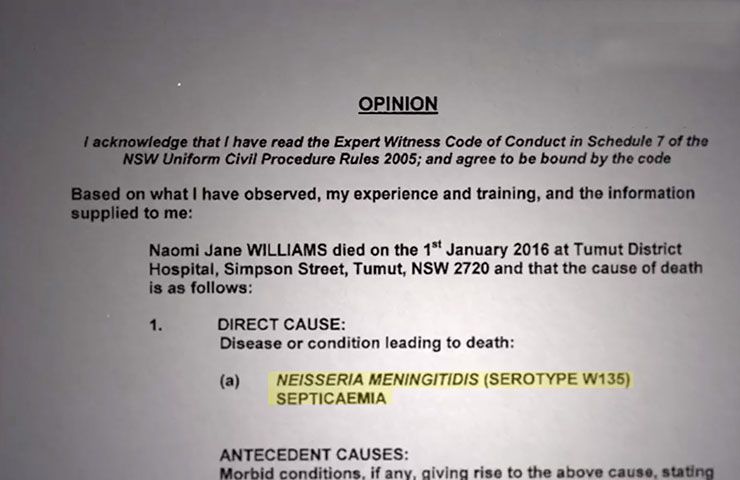
Everyone involved was shocked when Williams and her unborn baby passed away in the back of that ambulance. How could an otherwise healthy young woman like Williams suffer from a cardiac arrest and die en-route to the hospital? That question was on the lips of everyone concerned as an inquest into her death was opened immediately by medical staff at the hospital.
Conflicting Evidence
While it’s clear to all that Williams died as a result of the sepsis, the question remains about her manner of death and how serious a condition she was in when she first arrived at the hospital the night before. Counsel assisting the coroner, Lesley Whalan SC, outlined the nurses’ records of the incident in court, noting that they had written that the patient “looked well” during her first visit to the emergency room.
Vital Signs
As is standard practice, Williams’ vital signs were monitored when she arrived at the facility. She did show an elevated pulse, but everything else seemed to be completely normal and in order. She took some paracetamol and just 15 minutes later her blood pressure had returned to normal levels. They noted that the patient had been happily chatting and joking with staff and was pleased to be told she could go home.
Non-Urgent Presentation
The nurses’ records were robust enough to show that Williams visit to the emergency room that night suggested, “a non-urgent presentation for mild symptoms of generalized aches and pain, any abnormality in vital signs lasting no longer than 15 minutes,” according to a report in The Guardian. But there was a big discrepancy between that report and the symptoms her partner Lampe had noted. There was also text messages from Williams to her friends expressing worry and concern about the way she was feeling.
Needing Help
In one of those text messages, which were revealed as part of the inquest into the death, Williams sent a friend a message asking: “You wouldn’t be able to get me to the hospital, would you? I can barely move.” That friend was out of town however and suggested that Williams call an ambulance even if she couldn’t afford it. “Just my body aching all over, all good I’ll get there. Thanks anyway,” Williams texted back.
Numerous Visits
It came out as a result of the inquest that Williams had paid a visit to the hospital on an emergency basis 18 times over the past eight months. It even took Whalan a good 30 minutes to outline all of Williams’ presentations at the hospital. She was suffering on an almost constant basis from vomiting, nausea, and abdominal pain. In almost all of the cases, she was given anti-nausea medication and fluids, none of which solved the problem.
Testing Positive
Back in June, during one of her numerous visits to the emergency room, Williams tested positive for Helicobacter pylori, a stomach bacteria that causes pain and nausea. The doctor at the time recorded the cause of the bacteria as “unknown,” but she was also diagnosed with hyperemesis gravidarum, also known as extreme morning sickness. A few days later and Williams’ mother Sharon wrote to the head of the nursing staff at Tumut Hospital requesting a “specialist referral” for her daughter, but to no avail.
Not Addicted
For whatever reasons, the hospital staff put Williams’ condition down to drug or possibly alcohol addiction even though she had no issue with either. As Whalan explained to the inquest: “[Sharon] advised that her daughter was repeatedly referred for drug and alcohol counseling and this was adding to her daughter’s stress.” But a few months later and Williams was referred to Canberra Hospital as a “high-risk pregnancy.”
Proper Care
The inquest asked a lot of questions including whether or not Williams received the proper antenatal care she needed and why she wasn’t referred as a high-risk pregnancy early on. Whalan asked if it had anything to do with the fact she was of Aboriginal descent. Now some very uncomfortable and potentially damning questions were being asked, and people wanted answers.
Different Outcome
Whalan asked the people present at the inquest rhetorically: “Had Naomi been clearly identified as a high-risk maternity patient, either at the time or much earlier in her pregnancy, would events have unfolded differently from the early hours of January 1?” The fact that the bacteria that killed Williams could have been easily treated with antibiotics just compounded matters further.
Clinical Signs
The inquest heard that as Williams was a pregnant indigenous patient, she should have been considered as being a “high risk of sepsis.” Whalan then needed to look at whether those signs of sepsis were present when she visited the emergency room for the 18th time. On that day, Williams was neither vomiting nor was she dehydrated, unlike her previous visits. This, in turn, produced even more questions for the inquest.
Understated her Condition
The issue Whalan wanted to get to the bottom of was surrounding whether Williams let hospital staff know just how unwell she was feeling on the day when she arrived at the hospital. Could it be that Williams was just a bit of a trooper and decided to joke around with the nurses at the time instead of telling them how awful she felt for so many months? According to Whalan, that could have been the case.
Feeling Unwell
“Questions arise about how Naomi’s physical presentation was assessed given the absence of vomiting and dehydration when those symptoms had been present and severe on so many previous times,” Whalan said. “The question also arises as to whether Naomi herself, although feeling unwell, understated her condition or did not assert how unwell she was feeling at the time.” There is, therefore “substantial evidence” to Whalan’s mind that the staff at the Tumut Hospital failed to take Williams’ condition seriously enough.
Always Smiling
A close friend of the deceased, Talea Bulger, spoke to reporters following the untimely death of Williams. She said that Williams was the type who “always brought a smile to your face.” And it could have been Williams’ demeanor with hospital staff that was partially responsible for her death as nurses just assumed she was enduring a tough pregnancy and would be OK at the end of the day.
Deserved More
Bulger also spoke about how outraged she was, among other people, who felt that Williams simply didn’t receive the medical care that was due to her. “She was just a very happy, healthy, outgoing person until all these sicknesses started happening. That’s why we’re here, to figure out why she wasn’t given the treatment she deserved,” said Bulger.
Not Fair
Williams’ godmother, Sonia Piper, also spoke to the press about the loss of her goddaughter, explaining that she felt she received inferior medical care due to the fact she was Aboriginal. “I wouldn’t like this to happen to any Aboriginal people ever again because a lot of our people are dying out … and we need the care. And I think we’re entitled to the same as the non-Indigenous people,” she said.
Negligent Care
Piper continued: “I keep saying to everybody, why wasn’t she sent to a specialist somewhere in Sydney or Canberra? To really find out what was wrong with her? Because they were just giving her Panadol and sending her home. And if that poor woman was vomiting all the time and being sick, what was that doing to that little baby inside of her?” But tragically, Williams didn’t receive the medical care she needed, and many are now claiming she was treated negligently.
The Future
This tragic case highlights the difficult situation faced by many indigenous people in Australia. Coming from a lower socio-economic background than white Australians, Aboriginals have faced discrimination on many different levels over the years; including education and healthcare. As Piper concluded: “Something should be done. I don’t want to see this happen to any of my people. As an Aboriginal person and an elder of my community, I don’t want to see this again ever in my life.”